Report of Liberia Campaign November 2018
INTRODUCTION
The Liberia Campaign was proposed at the end of 2017 by the Cirujanos en Acción Foundation and without any doubt it has been a challenge and a great effort during the previous months, as we had to overcome difficulties in the recruitment of voluntaries, logistic problems as obtaining a large amount of medical and surgical material necessary for our work as the Ganta Hospital lacks all necessary means. The initial budget was very high with the visas, flights, life insurance, lodging and food for the whole team, the voluntaries themselves, the Cirujanos en Acción foundation and the donation of the Fundación Navarra “MuchosPocos” made up by workers and the Direction of the engineering firm M. Torres, a great example of social corporative responsibility. Transportation and the compulsory medical registration compulsory in Liberia were taken up by the Ganta Hospital.
Liberia is a country in Africa’s west with a 4,5 million inhabitants; its capital, Monrovia, has 1’15 million inhabitants; 84% live under the international poverty threshold (less than 1,25$ per day), and it occupies the tenth place in the poorest countries on earth, with an annual rent per capita of 683 $. The greater majority of its population is Christian (85’5%), and English is the official language, although 16 other languages are spoken. Its legal course coins are the Liberian dollar (1 LRD = 100 cents) and the American dollar, only banknotes. 5% of its population is made up from 2003, although its social and economical by “americo-liberians” or “congos”, descendants of liberated old slaves for the United States, and 95% are Africans from diverse ethnic groups.
Their recent history included two civil wars (1989-2003) with the result of 200.000 dead and 1 million refugees. At present there is peace from 2003, although its social and economical recovery was threatened by the largest epidemics of Ebola (2014-2015), in which more than 4.500 persons died, 300 of whom were doctors.
Ganta City is a place in the Nimbacounty, 5 hours from Monrovia, the largest and more populated of Liberia. The largest majority of its people live in miserable dwellings. The access to Gantha is by a road, recently constructed by a Chinese firm, and it takes 5 hours from the airport.
VOLUNTEERS
This has been the fourth Campaign in Ganta City, after the one organized by a Hernia International team in July 2017 by a Hernia International team, and two more later by the teams of Dr. David Fernández Luengas in September 2017 and Dr. Cesar Ramirez in April 2018, both from the Surgeons in Action Foundation. This is a humanitarian service with great medical needs and with the organization and collaboration of local people.
We seven volunteers belonged to the Fundación Cirujanos en Acción, and we come from México DF, Madrid, Segovia and Navarra:
· General Surgeons
o Dr. Manuel Cires Bezanilla, Estella Hospital, Navarra (Team Leader)
o Dr. Sandra del Barrrio Anaya, General Hospital of Segovia
o Dr. Estefanía Villalobos Rubalcaba, Medical Center ABC, Mexico DF
· Paediatric Surgeons:
o Dr. Lola Delgado Muñoz, 12 de Octubre University Hospital, Madrid
o Dr. Jesús Redondo Sedano, 12 de Octubre University Hospital, Madrid
· Anesthetists:
o Dr. Fabiola Ortega Ponce, Medical Center ABC, México DF
o Dr. Inmaculada Lahoz Jimeno, 12 de Octubre University Hospital, Madrid.
In collaboration with the “E&J Medical Center”, which helped in the surgical, hospital and consultation areas, I want to underline its capacity for work and collaboration. It has only three specialist doctors, Dr. Peter George, medical doctor and specialist in Ginecology and Obstetrics, who helped our stay, even if we hardly met him during our Campaign, De. Abenago, anaesthetist, and Dr. Jonas, General Surgeon, helped by Jhonson, anaesthetist technician and four nurses and helpers, Ruth, Othelo and Leon, as well as nurses and helpers in consultation and hospital work.
We carried 300kg of medical-surgical material in 12 large parcels, each prepared by volunteers in their hospitals; and controls at the Madrid-Barajas airport were made easy by the kind staff of the KLM; in the Monrovia Airport we were helped by the customs officials and the collaboration of the staff hired by Ganta Hospital staff for shifting our luggage and for going to Ganta in two vehicles with the kindness of its driver Junior.
The campaign lasted from 2nd to 10th November 2018. On Friday 2nd we started from Madrid for Monrovia via Amsterdam in the KLM airline, and we then were taken to Ganta city in a van; on Saturday 3rd we were given a warm welcome by the patients and staff of the Hospital in pure Godspel stile; we visited the different facilities of the Hospital and two work groups were established, one for the evaluation of the selected patients, and another to put in order and to classify all themedico-surgical material as well as the organizing and preparation of the four surgical rooms.
On Sunday 4th and till Thursday 8th we carried out five intensive surgical sessions from 8th to 19th, together with the daily visit to patients already upon and the evaluation and selection of new patients. Finally on 8th Friday we carried out our last visit, dismissed all the patients already operated upon, and attended the touching farewell of the hospital staff and patients. Then came our travelling back to Monrovia and arriving on Saturday 10th in Madrid.
Apart from the intense activity in the hospital which took up a great part of our time, we met in the Jackies Guest House, a simple hotel but with good cleanness and safety. It has a wifi net an a supermarket. We met there with people from other international organizations. Still, its high prize (50 shilings per room daily) apart from the breakfast and supper price rises heavily the campaign budget. Perhaps another cheaper place should be sought.
E&J Medical Center
It has a basic Laboratory, pharmacy, rooms for adults and paedriatics, urgency room, delivery room and two operation theaters. It has very limited means, and it makes up its deficiencies with the abundant material we brought with us like gauze, compressed, surgical gloves, exploration globes, dressing, sterile gowns, anaesthetics polietilen mesh (supplied by Hernia International Foundation) and antiseptics, suture instruments, electrical scalpel and its slab among other things.
It is necessary to mention that without this material it would be impossible to carry out a campaign in Ganta or in any other humanitarian place; if we consider the large number of interventions carried out we can see the large amount of material needed. We could perhaps think whether it would be better to buy the necessary material in the place of work, thus avoiding the difficulties of its transportation, the customs control, and ever growing difficulty of obtaining such things in our hospitals.
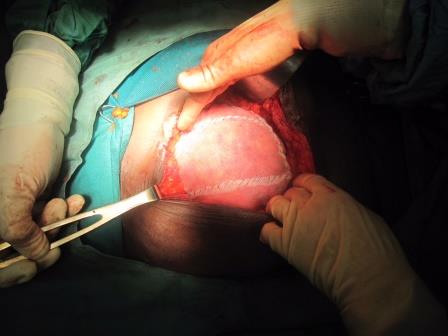
SURGICAL AREA
The surgical activity took place in four rooms, three for adult surgery and one for paediatric surgery.
Two rooms belong to the surgical aria of the Hospital: there is question of two basic operation rooms which an unusable room, as there is no oxygen neither anaesthetical gases. They do have two rooms in the surgical area of the Hospital, there is question of two basic operation theaters which have a not usable anaesthetics material as there is neither oxygen nor anaesthetical gases. They do have concentrators of oxygen and basic monitorization systems (blood pressure, heart frecuency and O2 saturation). They have their own electrical scalpel generator and operation theater tables and proper lights: although electric power is relatively stable,it is indispensable to have light source on the forehead to help. The paediatric and general Surgery worked in this area.
The other two surgical rooms were put up in two small rooms with very elementary means and surgical instruments; two electric scalpel generators belonging to the Surgeons in Action Foundation and insufficient head light depending always on our front lamps.
There are several batches of surgical instruments in acceptable conditions. We brought surgical instruments for adults as it is absolutely necessary if we want to work on a high number of patients.
Sterilization of material is carried out in an elementary autoclave. We used disposable surgical cloths as they hardly have any gowns or surgical cloths.
ACTIVITY
Number of procedures:
210 interventions during the campaign (more than 40 interventions per day).
80 interventions in child surgery
· 61 M, 19 F
· 51 inguinal hernias
· 24 umbilical hernias
· 5 others: circuncitions, hydrocele, haemangioma
· More frequent technique: intracanalicular
· General anaesthesia: Ketamine
130 interventions in adults surgery
o M 92; F 38
o 95 inguinal hernias (70 M; 25 F)
o 19 umbilical hernia ,
o 11 epigastric hernias
o 5 Others: femoral hernias, angioma, apendicitis, suprapubic catheterization, retirada de malla por rechazo
o More frequent technique:
Hernioplastic of Lichtenstein.
o Epidural anaesthesia
BUDGET:
The Ganta City campaign has a budget higher in comparison with other places, due to the high cost of the VISA, airfligth ticket, lodgin and maintenance.
In the budget we have not taken into account the cost of the surgical material, contributed by the volunteers.
TOTAL COST OF THE CAMPAIGN (VISA+AIR TICKET+HOTEL+MAINTENANCE): 11.000€
COST PER VOLUNTEER 1500 €
Dr. Manuel Cires
Leader of Ganta City Campaign
Surgeons in Action Foundation