KAMUTUR SURGICAL CAMPAIGN. BUKEDEA DISTRICT. UGANDA. SEPTEMBER 20th-30th 2019
SURGEONS IN ACTION FOUNDATION

1.TECHNICAL REPORT:
a. DATE AND LOGISTICS:

A team of 12 people: 4 general surgeons, 1 pediatric surgeon, 3 anesthesiologists, 1 radiologist,
two surgical nurses and a professional photographer.18 packages with a total of about 400kg ofsurgical equipment and medicines.

Departure from Madrid on Friday 20/9 at night and arrival in Madrid on Monday 30/9 in the morning.
This time we traveled with Ethiopian Airlines. A success, because the journey, with stopover in
Addis Ababba, is shorter, and also allows us to carry 2 23kg packages per person.
Saturday 21/9: A long bus journey, which we already know from other campaigns, heavy due to
long distance and what it means to travel on the road through Africa: traffic jams, pavement in bad
condition, dirt tracks.., until reaching Kamutur, a village in a rural setting in the Bukedea district.

Sunday 21 to Friday 27/9: Surgical interventions, from 8:00h to 20h, in 3 simultaneous operating rooms.
b. ADULT PATIENTS:
68 procedures have been operated on in 62 adults.



More complex procedures have been performed than in previous campaigns, thanks to improvements made
in the new surgical ward. To highlight some procedures:
-19 inguinal hernioplasties, with PLP meshes provided by the volunteers.
-1 infraumbilical laparotomy for removal of right ovarian cystic mass, previously
diagnosed by ultrasound by our radiologist.
-1 xyphopubic laparotomy for massive splenectomy.
-8 hemitiroidectomies by unilateral giant goiters.


-1 total thyroidectomy per giant bilateral goiter.
-3 large submandibular pleomorphic adenomas.
-1 large left inguinal tumor with extension to the thigh, about 20cm, Schwannoma said by pathology
report.
-1 large incisional hernia, with retromuscular PLP mesh (Rives)
-The rest of procedures have included umbilical hernias, anal pathology, soft-tissue
tumors (some of them very large) and removal of complex keloid scars.
c. PEDIATRIC PATIENTS:


35 procedures have been operated on in 25 paediatric patients, from 1 to 16 years of age. As most
noteworthy:
-7 inguinal hernias-4 hydroceles
-1 retrorectal teratoma.
-1 patient of 16th with multiple neurofibromas in left face, of great complexity, who had been
abandoned in the hospital.
-1 distal hypospadias.
-All other procedures include umbilical hernias, cures and soft-tissue tumors.


We have had to reject some paediatric patients, because of high complexity, such as a large facial
tumor, stoma closures or tonsil surgery.
It should be noted that, due to the location of the hospital in a rural environment, away from any
urban core of a certain entity, the recruitment of patients is quite complicated. Firstly, because
of the campaign’s publicity difficulties (advertinsingsare placed on local radio stations and phone
messages are sent) and secondly because of the patient’s difficulties in getting to the hospital.
This is especially sensitive for paediatric patients.
Total procedures: 103
Total patients: 87c. COMPLICATIONS:
So far as to leave Kamutur on Saturday 28/9 in the early morning, it is worth highlighting only two
re-interventions by post-surgical hematomas, one in total thyroidectomy, which was successfully
resolved, and another after removal of a pleomorphal adenoma submandibular, equally resolved with
drainage. We haven’t had any phonatory complications in any thyroidectomy. The patient who had
splenectomy was pending post-splenectomy vaccination,and has evolved successfully following our
departure. The pediatric patient with face neurofibromas has successfully evolved with healing of
the surgical wound, keeping important palpebral oedema that evolves more slowly (one of the removed
neurofibromas was in retroorbital location). The rest of the patients have had no complications.
We have received reports of Pathological Anatomy from Mbale Hospital, of the cases we consider most
necessary. For subsequent campaigns, always assessing the difficulties and cost of this, let it
be known that this study can be carried out in the samples deemed appropriate.

2. CAMPAIGN REPORT
a. THE PLACE:
Uganda is an East African country, bordering Kenya, South Sudan, Congo, Rwanda and Tanzania. It is
an independent country, belonging to the Commonwealth, since 1962. He has had a very convulsive
recent past, and currently maintains a relative socio- political calm, with presidential regime led
by Museweni, who has ruled since 1986. It is divided into 111 districts and a capital city,
Kampala. More than 80% of the population is Christian. Each woman has an average of more than 6
children. Life expectancy is estimated to be around 52 years. The Bukedea district, where Kamutur
is located, is a district with about 120. 000 hab, in a rural environment, and with 80% of itspopulation below the poverty line.

The Holy Innocents Health Center (HIHC) has improved a lot since our last visit. It currently has
care for gestation and delivery, hospitalization area, laboratory with basic diagnostic tests,
and a surgical pavilion already completed, and a new surgical hospitalization building connected to
the surgical pavilion, in a very advanced phase of construction, with a ward for women and another
for men.
Regarding the surgical pavilion, it is a building that has 3 operating rooms, whose current
endowment is:
-1 operating room with electro-surgery generator, an anesthesia tower and a monitor.
-1 operating room with an electro-surgery generator, a monitor and an oxygen concentrator.
-1 operating room without electro-scalpel.
All three operating rooms have a new and very functional operating table. There are legs. Each has
ceiling light and a floor lamp, although it is advisable to bring front spotlights.
There is no running water yet available, although it appears that the external pipeline from Mbale
will be completed in the coming months.
In addition to operating rooms, the pavilion has toilets for men and women, a post- anesthetic
recovery room, a cleaning room, an instrument and sterilization room, a warehouse, a staff room
and a waiting area for patients.
It has a system of solar panels and rechargeable batteries to support electric power.
Unfortunately, it is still not enough to meet the needs of the pavilion when it is operating at
full capacity more than two days, because the rate of charge of the batteries is lower than the
consumption rate, so it is necessary, to this day, to complement the energy input with a diesel
generator. This situation is likely to change with improvements that are pending, one is the
increase in battery capacity, and the other is the arrival of power supply that is planned for theend of this year.

The hospital center is clean and tidy. A more than acceptable asepsis-antisepsis circuit is
maintained, using a pressure autoclave using a gas-heated pot (there is an autoclave, which
consumes too much electrical energy and cannot be used at the moment) and organizing the instrument
in small kits, aided by all the single-use sterilized material we carry with us. We have
collaborated with 3 very efficient and willing local nurses, to which we appreciate their great
capacity and willingness to work.
With regard to the admission process, two aspects should be highlighted:
-The admission process in the hospital includes the payment of between 10,000 and 50,000 Ugandan
shillings, which is equivalent to a maximum of 12 euros, and the completion of a small medical
history by local doctors, usually in the days before our arrival.
-The medical team of the campaign consulted in the consultation area all the selected patients, to
decide the indication and order of surgery.
It should be noted that any surgical intervention in Mbale Hospital, especially in the case of more
complex patients such as thyroidectomies, can account for between several hundred thousand and
several million Ugandan shillings. Apart from some cases where the indication of surgicalintervention by the surgeons responsible is not accepted.

b. THE TEAM
On September 20, Friday night, we left Madrid a team of 12 people:
-Carlos de la Torre Ramos, pediatricsurgeon,
-Sebastián Fernández Arias, general surgeon,
-Ana Gay Fernández, general surgeon,
-Julio Calvete Chornet, general surgeon,
-Beatriz Revuelta Alonso, anesthesiologist,
-Miguel Angel Pereira Loureiro, anesthesiologist,
-Astrid Alvarez Fernández, anaesthetologist in training (R4)
-Nieves Alegre Bernal, radiologist,
-Nuria Agulló Marin, nurse,
-Gustavo Sánchez Bravo, nurse,
-Sergio Sánchez Agulló, photographer,

-David Fernández Luengas, general surgeon.
This campaign has been carried out by a team from the Surgeons in Action Foundation. Together with
the medical team, on this occasion a professional photographer has participated in the campaign,
with the aim of collecting audiovisual material to make a documentary montage about this place, its
reality, its needs, and the task that the Fundación Action takes place here.
c. LOCAL STAFF
There are currently two doctors at the hospital. For our work, we have had 2 nurses in the
operating room (Esther and Rose), who did circulating work together with our nurses, and cleaning
and sterilization. In addition, we work with hospital nurses, who assist all hospitalized patients
24 hours a day, and two wardens who take care of patient transport and other tasks. It is right
to acknowledge to all of them the enormous effort made and the joy with which they have shared the
work with us. We were very pleased to note upon our arrival the cleanliness of the facilities,
which we were able to check how it was maintained day after day by the cleaning team.
We have also collaborated with local doctors (Viktor and Kenneth), who have helped us with the
prior selection of patients, and have participated in surgical interventions. During the last day
in Kamutur, there was a great celebration, on the occasion of the official opening of the
surgical pavilion. More than 100 people attended, with the presence of Ugandan Senate
authorities, representatives of the Ministry of Health, and the Bishop of Mbale. A mass was
officiated and the pavilion was officially opened. The authorities present were able to check the
enormous effort made to equip the hospital with the necessary means to perform surgical interventions safely.
d. THE EQUIPMENT
In addition to the surgical ward, it is worth noting:
-Surgical instruments, there is a basic reserve of instruments in the hospital, but we have carried
instrumentals to make about 6 basic kits, which have allowed us to work fluently, relying on
constant cleaning and sterilization in the autoclave by local nurses.
-Regarding consumable material and operating room clothing, the needs are enormous.We have used
much of the material we have worn, among gauze, compresses, gloves, dressings, disposable sterile
cloths, disposable sterile gowns, anesthetic medication iv, iv antibiotics for prophylaxis,
mosquito meshes and antiseptic solutions for surgical wash, among other things. Without this
material, posing such a campaign to this place is impossible. The next teams must be very aware of
the need to provide all this material, although it is true that, thanks to the material left over
from previous campaigns, material is gradually stored in the pavilion (current inventory of the
warehouse is attached).
-Regarding the work of our radiologist, she has been able to use a simple ultrasound, acquired by
the hospital, which has a single low frequency convex probe for abdominal cavity examination, and
does not have Doppler. With it she has carried out two different tasks:
1.- Diagnostic studies to the patients we have required.
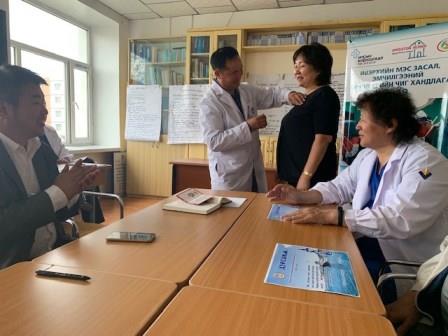
2.- Basic training plan in the use of the ultrasound for doctors and local midwives, for use in
basic diagnostic studies and for gestation control.
-Another task that we have done during the campaign is the training of local staff in basic
cardiopulmonary resuscitation maneuvers, with a CPR mannequin donated by the company Ambú, and which we have left there so that in future campaigns you can continue to use
it for training.
e. ANESTESIA, ASEPSIA AND QUIRURGIC MATERIAL

1. Anesthesia: The hospital has an anesthesia machine and an oxygen concentrator. The anesthesia
machine functions as an oxygen concentrator, i.e. it collects ambient air and concentrates it to
get Fi02 of approximately 80-90%. It could be connected to an oxygen bullet or a wall oxygen
delivery system, but the pavilion lacks these systems. Yes there are a couple of oxygen bullets,
but the connections are not compatible and their use would leave the hospital without them, so the
bullets were nearby to use only in case of urgency. The respirator has an internal battery that
lasts about 30 minutes, to take into account in case of failure with generators or solar panels.
The oxygen concentrator continues to function perfectly, so we were able to perform general
anesthesia in two of the operating rooms simultaneously.
In the third operating room, most surgeries were performed under local anesthesia and many with
locorregional anesthesia, without incidents.
In this campaign, thyroid surgery was done for the first time, with everything surrounding these
types of interventions. In addition to the laryngoscopes, we had fasteners and we carried airtraq
of different sizes. We used them in a timely manner, but all the orotracheal intubations were
successful, without any incident. Although if such interventions are to continue, we must be prepared for possible difficulties.

In addition to all the medication usually carried in these campaigns, the Hospital was insisted on
the provision of halothane (there is only one halothane vaporizer, it is not possible to use
another type of gases), to be able to perform the maximum number of surgeries with the lowest cost
in inductors, and some kind of muscle relaxant. In previous campaigns there was no fridge to store
the medication. Now there is a fridge in the surgical pavilion, and we got succinylcholine and
cisatracurium in Kampala, albeit at a very high price. Halothane is almost impossible to obtain
in European countries, and in Uganda they can take care of buying it. The relaxants should take
them, so in future campaigns it would be possible to carry what each anaesthetist considers, well
protected in cold during the trip, since there they can be stored without problem.
With regard to the material they have in their warehouse, there is a significant surplus in face
masks, guedel, spinal needles of different sizes, local anesthetics (hiperbara and and isobara
bupivacaine), electrodes, nasal oxygen masks. All other medications and fungibles need to be
provided in each mission. Important mention of any drug we anticipate needing in thyroid surgeries.
For this campaign we have carried calcium gluconate iv, calcium+calcitriol oral, levothyrosine, as
well as material for eventual realization of tracheostomies.
Surgery was performed in adults (abdominal wall, thyroid, skin tumors…) and in children
(abdominal wall, urological, sacrocoxygeal, facial tumor…) without any incidenceof any kind.
2. Asepsis: Basically, they have a “sterilization” room where they store the packages with the
sterile material, and where a “express pot” autoclave is placed on gas fire, with pressure meter.
The system itself is rudimentary, but effective for getting the material sterilized. I
recommend the following teams to carry sterilization bags and witnesses, very useful there.
Surgical clothing is very scarce, with very few cotton gowns and re-sterilizable cloths. We use a
lot of disposable cloths that we carry from Spain, as well as disposable robes. We have been
particularly concerned that all our adult patients with indication of antibiotic prophylaxis
receive a dose of cephazoline 2gr iv or similar in anesthetic induction, which we have taken. In
the hospital there is a pharmacy with some medications, but in general, it is advisable to take all
the medicines that are deemed to be used.
3. With regard to surgical equipment, we carried a lot of material that is essential that other
missions also carry, from gauze and compresses to sterile gloves, drains, dressings, steri-streaps,
sutures, elastic bandages, etc…
The surgical instruments there are useful, although generally somewhat rudimentary. We have
preferably used our own instrumental divided into small kits.
f. OUR LIFE IN KAMUTUR
The alarm clock rings at 7:00am. It’s time to get up, grab a big bucket and approach the hospital
well, in the middle of the central square to fill it with water. There’s enough hustle at that
time, and you always find some kid in the well that gladly applies to the pot’s crank to get the
bucket filled. Then there is going through the kitchens to add enough hot water, for tastes, and
approach our “shower”: a stay with walls of approx. 1.5m high, outdoors, where we could perfect the
technique of the bucket shower. The mornings are fresh, about 20 degrees max. The rest of the day
during this time of year is warm, up to 30 degrees, and with relatively frequent rain showers. As
far as the bathroom is concerned, we have improved from last year. It is no longer necessary to go
to the latrine “communal”, because we have a bathroom in the area of the bedrooms and two others in
the surgical pavilion. As there is no running water, it is necessary to pour a good bucket of water
for flushing the toilet.
All meals were made on the covered terrace, with a menu basically the same every day, clean, cooked
there, and enough to feed, without great difficulties.
Our life in this place is very simple. We have always felt very well treated and very accompanied.
Apart from hospital life, which occupied much of the day, our social life was limited to
conversations around the table. Especially in the evenings, when, after dinner, we enjoyed one (or
two) wonderful bottles (75cl) of Nile beer, with an entertaining conversation.
Regarding the rooms, we have lived in relatively cozy cabins, two for the 6boys, another for the 4
girls, and a room for Nuria and for me. They are quite basic, with the beds as only furniture, but
clean and comfortable enough to spend a week.We paid around $70 each for the room and food, for the
whole week.
Communication with the outside world can only be done through the Ugandan telephone network, via
SMS or calls at an international rate.
Our trip back to Entebbe we did it in two days of car of about 4.5h each day, taking the time to
rest on Saturday in a hotel in Jinja, where we could enjoy a boat ride on Lake Victoria, visiting
the famous source of the river Nile.
3. CONCLUSION:
In short, we consider that this campaign has been a success, both for the number and complexity of
patients that we have been able to operate, with little complications, and for the satisfaction of
the team for the great treatment received by the authorities and local staff. This year, thanks to
the functioning of the pavilion, we have been able to perform, for the first time in Kamutur, surgical interventions of greater complexity, with general anesthesia, such as thyroidectomies and abdominal surgery.
Strengths of this place:
– Moses Aisia, true hospital engine. Its ability to launch, from nothing, this center, is amazing.
– The hospital itself, a true center of hope for this place, with a much-needed population, mired
in poverty.
– The treatment we have received and the willingness of the staff to work with us.
– The works carried out, with the surgical pavilion already functioning, and the new
hospitalization ward in the very advanced phase of construction.
Improvement objectives:
– Improve the process of recruiting patients for campaigns. This is a goal that should be
considered paramount, to make the most of campaigns. Among the measures that can be implemented,
there are two that would probably be very profitable:
-Get a means of transport that would collect patients in nearby villages in the days leading up to
the campaign.
-Make a visit to Kamutur Elementary School, which has 681 students censed today, to perform a
medical checkfor surgical pathology, which is likely to be going unnoticed to their parents.
– Ensure complete energy independence in the surgical pavilion.
– Medical material: Today, any campaign must have the need, already explained, to carry with all
necessary medical material. Our recommendation is maintained to supply the hospital with this
material, by the management of the center.
– Complete the channelling of running water and electricity, by the Ugandan government.
– Complete the start-up of the blood bank, currently in the manning phase, according to the rules
of the control protocol required by the Mbale Blood Bank.
4. BUDGET:
For informational purposes, and without going into excessive detail, it must be said that the
campaign in Kamutur is more affordable for the surgical team than other locations. This is due to
two fundamental reasons. One, the cost of the plane ticket, not especially expensive. Another, the
costs of accommodation and maintenance, which have been almost non-existent (70$ for the entire
stay of 6 days), in addition to road transport, about 450 dollars round trip all the equipment. The
budget has not accounted for the cost of all the material we have contributed, in total about
400kg.
COST PER PARTICIPANT: Approx. 900€
TOTAL COST OF THE CAMPAIGN: Approx. 10,800€, paid for by the volunteers and with partial funding
thanks to the Spanish Surgical Association grant of 3500€.
Fdo.: David Fernández Luengas Responsible for the campaign
Surgeons in Action