MIXED ABDOMINAL WALL SURGERY AND VASCULAR SURGERY CAMPAIGN
DATE: 15 to 29 September 2024 – VENTANILLA HOSPITAL/CALLAO/PERU

Contents
1. TECHNICAL REPORT: 1
2. CAMPAIGN REPORT 1
3. CONCLUSION 2
4. BUDGET: (small breakdown of expenditure) 2
5. SIGNATURES 2
1. TECHNICAL REPORTS:
1.1 DATES AND LOGISTICS DEPLOYED:

– On the 14th of September 2024 most of the Cirujanos en Acción team left Madrid for Lima at 5pm, bringing medical and biomedical material in sufficient quantity to cover the objectives of the campaign, as well as 2 diathermy generators from the Foundation
– On Sunday 15th September at 06:00 hours, the team arrived at Jorge Chavez Airport and was welcomed by a small local entourage. That same day, the evaluation of the patients began in the morning at the Ventanilla Hospital, by Dr. Concha Bernardos (Vascular Surgery) and Dr. Jose Maria Pérez Alfranca (General Surgery).
– Surgical activities started on Monday 16th September, as detailed below.
– The surgical activities culminated on Friday 27th September with a closing ceremony organized by the Regional Health Directorate of Callao.
– On the evening of 28 September, most of the team left Jorge Chavez airport for Madrid.
1.2 ADULTS PACIENTS:
During the health campaign, 159 patients and 193 cases were operated on. Of the total, 86 patients (93 cases) were treated for hernias and 73 patients (100 cases) for varicose veins in the lower limbs.
The type of intervention performed was hernioplasty and/or eventroplasty, with the polypropylene prosthesis being placed. In the case of umbilical hernias, the decision to use a polypropylene prosthesis was based on the size of the ring. The hernia pathology operations were performed in 02 operating theatres, with 2 anaesthesiologists and 2 surgeons in each theatre.
– Number of adults: 86
– Number of procedures performed: 93.
– Average number of procedures per day: 10.

With regard to surgery for varicose veins in MMII, phleboextraction of the internal saphenous vein was performed using the scripting technique in most cases. In the rest, external saphenous ligation or perforating ligatures were performed. In addition, phlebectomy of the varicose bundles was performed in all cases. Varicose vein operations were performed in 02 operating theatres, with 2 anaesthesiologists and 1 surgeon.
– Number of adults: 73
– Number of procedures performed: 100.
– Average number of procedures per day: 10.

1.3 PEDIATRIC PACIENTS:
It was not attended.
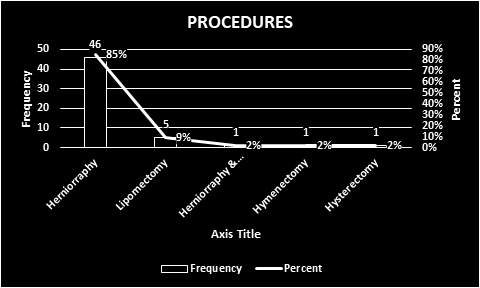
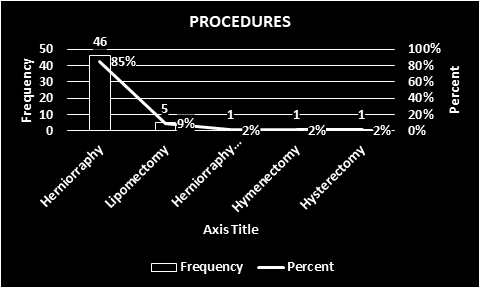
1.4 Total Procedures
HERNIAL PATHOLOGY:
– INCISIONAL HERNIA 6
– EPIGASTRIC HERNIA 4
– INGUINAL HERNIA 35
– SUPRAUMBILICAL HERNIA 4
– UMBILICAL HERNIA 44
TOTAL 93

VARICOSE VEIN SURGERY:
PHLEBOEXTRACTION OF INTERNAL SAPHENOUS VEIN 94 CASES
EXTERNAL SAPHENOUS VEIN LIGATION 4 CASES
PERFORATOR LIGATION 2 CASES
TOTAL 100

1.5 Total pacients
HERNIA AND ABDOMINAL WALL SURGERY: 86 PATIENTS.
VARICOSE VEIN SURGERY: 73
TOTAL NUMBER OF PATIENTS: 159.
1.6 COMPLICATIONS
Serious:
There were no acute complications during the first 24 hours post-operatively.
Recurrent:
As of today that we are in contact with Dr. VELASQUEZ to follow the evolution of our patients, we have not received any information of complications so far.
CAMPAIGN REPORT
2.1. THE PLACE
Last September, a new cooperation campaign took place in the district of Ventanilla (Callao – Peru). Ventanilla is located 34 kilometres northwest of Lima and is a coastal district with a constantly growing population of 355,830 inhabitants. Its main independent economic activity is commerce, ecotourism-recreational activities and, to a lesser extent, artisanal fishing.
The Ventanilla Hospital began its activities in 1964 as a health centre in a building on 12th Street in the Ciudad Satélite de Ventanilla housing estate. On 8 February 1967, it moved to its current location on block 3 of Avenida Pedro Beltrán, next to the Ventanilla Police Station. Since January 2013 it has functioned as the Ventanilla Hospital, with Dr. David Pablo González Sáenz as its first Director, and is currently under the direction of Dr. Hamilton Alejandro García Díaz.

Ventanilla hospital has 5 operating theatres, 4 of which were available for the campaign, initially 2 operating theatres for abdominal wall pathology and 2 operating theatres for varicose veins. The surgery area has an inpatient ward, which was used for patients who required monitoring for more than 1 day or for some particularity of the patient.
The recruitment of the patients took place a few days before the campaign and was carried out by the medical staff of the Ventanilla Hospital. On Sunday 15th September the patients were evaluated by Dr. Concha BERNARDOS (Vascular Surgery) and Dr. Jose Maria PEREZ (General Surgery). This evaluation consisted of prioritisation according to the patient’s individual situation and assessment of the need for surgical treatment.
The project of this campaign aimed to treat between 90 to 100 patients, at a rate of 15 to 20 patients per day. At the end of the campaign, 159 patients were operated on and 193 surgical procedures were performed.
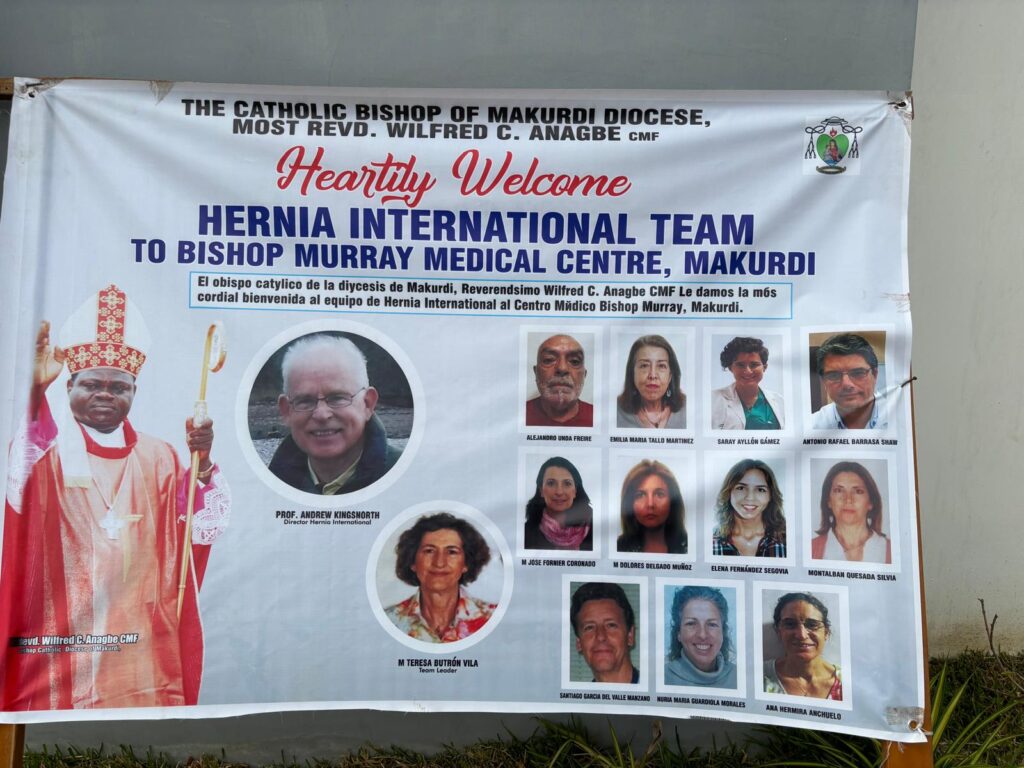
For this campaign we also had the support of Hernia International, who lent the Ventanilla Hospital four (04) boxes of surgical instruments, which made it possible to perform the surgeries continuously in multiple operating theatres.

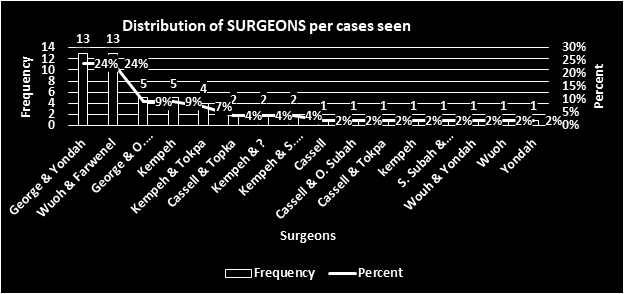
2.2. THE TEAM
The team of volunteers consisted of 5 general surgeons, 1 vascular surgeon, 2 vascular surgery residents, 3 anaesthetists, 5 nurses and a 3rd year medical student:
– A general surgeon from the Hospital Regional Policial de Arequipa (Dr. Ameth Alvarez).
– A general surgeon from Australia (Marisol Perez Cerdeira).
– A general surgeon from Spain (José Maria Perez Alfranca).
– 2 general surgeons from Lima (Roberto VEGA, Ronal Medina).
– A vascular surgeon from Spain (Dr. C Bernardos). Spanish team coordinator.
– 2 vascular surgery residents from Spain (Beatriz García Nieto and Alejandra Vázquez).
– 3 anaesthesiologists from Spain (Pilar Murga Pascual, M Jesús Sánchez Colomer, Fernando Carbó).
– 4 nurses from Spain (María José Fornier Coronado, María Jesús Nieto Berrocal, Lucía Ruiz Arasanz y Maria Alicia Zapata Piquer)
– 1 nurse from Arequipa (Giovanna Haydee Mesa Mendoza de Álvarez)
– 1 field worker in Lima (Martha Vasquez)
– 1 medical student (Paloma Baselga).
2.3. LOCAL STAFF
– 01 general surgeon coordinating recruitment (Dr. Velásquez)
– 04 general surgeons from Ventanilla Hospital (Bernal, Cutipa, Lavado, Huamani)
– 04 general surgery residents from Ventanilla Hospital (Alice Bada, Pedro Anderson, Mildret Rodriguez)
– Nurses and technical staff from the surgical centre.
2.4. EQUIPMENT
The following equipment was available for this campaign:
– 4 daily operating theatres with operation from 8-20h or until the schedule is completed.
– Anaesthetic recovery with 6 beds.
– An Echo Doppler for pre or intraoperative evaluation.
– 2 diathermy generators from Ventanilla Hospital and 2 diathermy generators brought by Surgeons in Action.

SURGICAL INSTRUMENTS
For the present campaign we had 4 boxes of instruments from Ventanilla´s Hospital and 04 boxes from Hernia Internacional, each box to be used and sterilised with a minimum content of:
- – 02 FARABEUF OR 2 ROUX
- – 10-12 MOSQUITOES
- – 2-3 CRYLES
- – 1 MAY SCISSORS
- – 1 METCENBAUM SCISSORS
- – 2 TWEEZERS WITH TEETH
- – 2 DISSECTING FORCEPS
- – 1 NEEDLE HOLDER
- – 1 SCALPEL HANDLE º4
- – 4 FLEBOEXTRACTOR CRABS AND HOOKS (brought by Surgeons in Action)
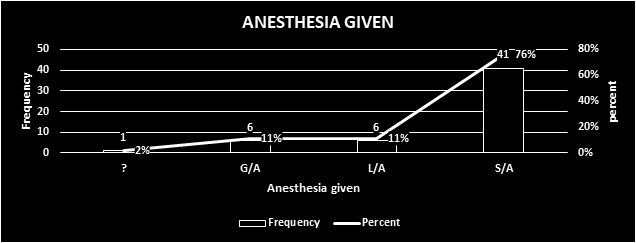
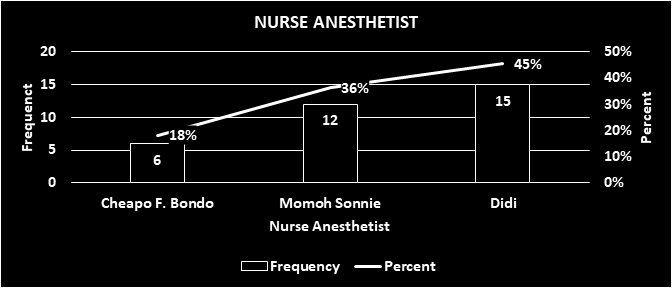
2.5. ANAESTHESIA
Type of anaesthesia used:
– SPINAL. 126 PATIENTS.
– LOCAL AND SEDATION 26 PATIENTS.
– GENERAL
3 PATIENTS

2.4. ASEPSIS AND SURGICAL SUPPLIES
The following surgical material was brought for this campaign according to the following list:
2.5. OUR LIFE ON……
The Ventanilla Hospital is located in the district of the same name, and it is a 50-minute drive from the Lauritas Sisters’ place of residence, Casa de reposo, to the hospital and back, in a vehicle available only to the team.
The month of September was cold in the mornings, which was the constant on arrival at the hospital. By lunchtime, which was at 02:30 pm, the weather changed to a little sunny, which improved our spirits..

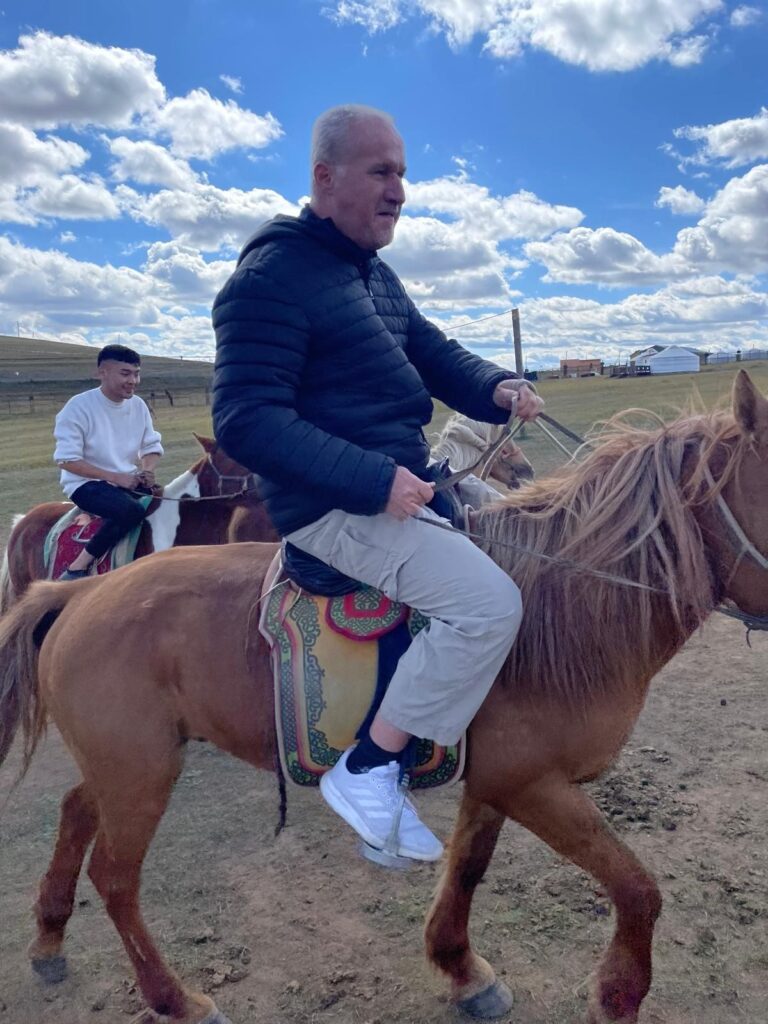
Between surgeries, there was always time to share with colleagues and also with the residents, who were the ones who gained the most interaction and experience during all the days of the campaign. At the end of each surgery, the feeling of satisfaction at having achieved the objectives of the campaign was evident in the team. The activities of the surgical act were not left aside, with the preoperative evaluation and the operative report being carried out by the surgeon in charge of the procedure. During the course of the campaign there were some pleasant moments not associated with the operating theatre, such as the visit of a dance group, who showed us a little bit of Peruvian folklore, making the surgical team participate in this activity, which was very pleasant for everyone. Also during the course of the campaign, Dr Roberto ESPINOZA ATOCHE – Regional Director of Health of Callao, visited us and showed his gratitude to the team for the activity, highlighting their generosity, solidarity and great surgical capacity.

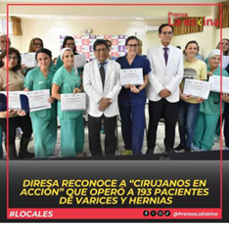
At the end of the campaign there was a closing activity, which was presided over by the Regional Health Director of Callao, with the presence of the Director of Ventanilla Hospital, in this activity once again thanking the selfless work of the team with the sole objective of improving the health of the people of Ventanilla most in need. The closing ceremony also included the presentation of certificates to the members of the Surgeons in Action team, a fact that was highlighted in the local media and virtual media of DIRESA Callao..
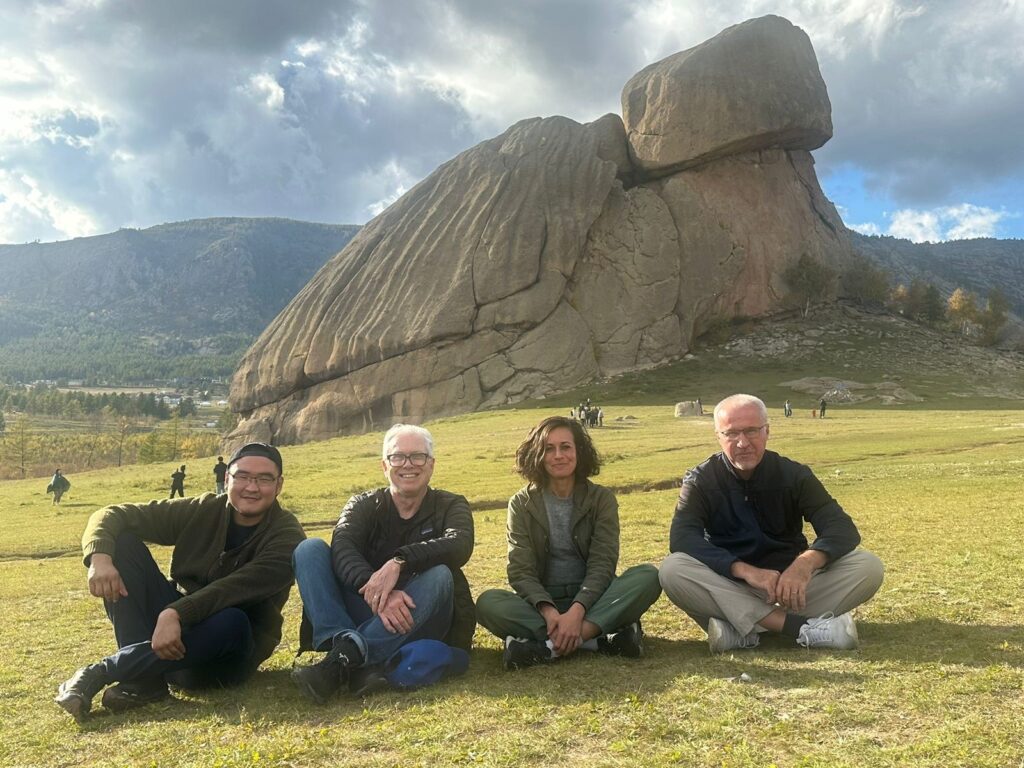
In the free time there was time to get to know part of Lima, such as the districts of Barranco and Miraflores, with all their architecture, culture and traditional food. There was also time to get to know a little more of Peru, with a short visit to Ica, Nazca and Paracas..
2. CONCLUSION

3.1 Strengts of this place:
– Ventanilla Hospital has 4 rooms available for campaigns, 2 operating theatres complete with anaesthesia machine and 2 smaller operating theatres suitable for low complexity procedures, which do not have electrocautery.
– Ventanilla Hospital has a dining room where staff can have lunch.
– The Ventanilla Hospital has surgical residents who are very supportive of the campaign.
– The nursing staff of the surgical centre has experience in conducting these campaigns, successfully managing the flow of patients in the surgical centre and in the hospital.
– Ventanilla Hospital has its own sterilisation centre.
3.2. Improvements objetives:
– Recruitment of patients earlier, for greater coverage.
– The leader of the local campaign team should be a surgeon from the hospital or centre where the campaign will take place.
– Manage the actual number of beneficiaries of the campaign in order to better distribute the patients and the surgical team.
– The location of the team’s accommodation should be closer to the place where the campaign will take place, in order to avoid transport time, which is made worse by the high traffic in Lima.
3. BUDGET: (small breakdown of expenditure)
4.1. COST PER PARTICIPANT:
Air tickets Madrid/Lima/Madrid, 800 ————————————– 800 euros.
Bus and taxi , 35 —————————- —————————————35 euros
Meals and accommodation per person, 100 euros /day (12 days) 1200 euros
Medical insurance including medical repatriation ————————–35 euros
Total expenses per participant ————————————————-2070 euros
4.2. TOTAL COST OF THE CAMPAING:
Fixed costs:
Medical equipment —————————————————————————–1,000 euros
Transport of equipment: – 500 kilograms ————————– ——————-500 euros
Transport of medical personnel:
11 plane tickets Madrid/Lima/Madrid, 800×11 = —————————————-8,800 euros.
Bus and taxi, 35 x 11 —————————–=———————————————- 385 euros.
Meals and accommodation – 11 persons, 100 euros person/day (1-2 days) —— 13.200 euros.
Medical insurance including medical repatriation. 35x 11 ———————— -385 euros
Total expenses: ———————————————————————————–24.270 euros
2. SIGNATURES
S.D:
Cirujanos en Acción
AMETH GALINDO ALVAREZ FLORES
CONCEPCION BERNARDOS ALCALDE