The Hernia International Meru camp was conducted over two weeks from November 4-15. This was a quickly organized trip that was coordinated with the help of Peter Karanje of Nairobi, Kenya with the support of the Ministry of Foreign and Diaspora Affairs that came together at the last minute.
The Team consisted of surgeons from the USA and Australia and an anesthetist from Australia. We collaborated with the Ambassador and staff from the Ministry of Foreign and Diaspora Affairs as well as local administrators and staff at the Meru Teaching and Referral Hospital.
- Heidi Miller – MIS/Hernia Surgeon – USA
- Cea-Cea Moller – General/Trauma Surgeon – Australia
- Chandra Hassan – Bariatric/General Surgeon – USA
- Dominique Roberts – Retired General Surgeon – Australia/France
- LiLin Hong – Anesthetist – Australia
- Peter Karanje – Businessman/Logistics coordinator – Kenya

There was very minimal pre-mission planning with the hospital which made for a slow start in our clinical activities, but this ramped up nicely. We were met at the hotel in Nairobi by Peter and the representatives of the Diaspora who provided our transportation for the two weeks of the camp. The trip from Nairobi to Meru is approximately 5 hours by bus and passes around Mount Kenya which was hidden in the rainy season cloud cover our entire trip. On arrival we settled into the Meru Slopes hotel, which was comfortable and walking distance to the hospital. The first morning we were met by the administrators, surgeons and surgical trainees and given a tour of the beautiful and clean grounds of the Meru Teaching and Referral Hospital. The hospital has a working ICU and dialysis unit as well as a maternity ward and theater. The Casualty is set up with Xray and a theatre, but it was not functioning due to staffing issues. The radiology unit consisted of ultrasound, CT and MRI although the latter two were both nonfunctional during our visit. In the case of a required CT scan for an incarcerated complex recurrent incisional hernia, the patient was transported to a private hospital and paid out of pocket to have this done.



The patients were evaluated by the surgical trainees and admitted the day prior to their surgery dates. Our OR lists were completed the day before and we operated Thursday and Friday the first week and Monday through Thursday the second week. We used a combination of pure local, local with sedation, spinal and general anesthesia. Dr Hong oversaw a lot of the anesthesia care, but this was also supported by local providers. We cared for a total of 35 patients aged between 2 and 78. We fixed 17 inguinal, 8 umbilical, 12 epigastric and 2 recurrent incisional hernias. We also saw 12 patients in consultation during a Tuesday clinic afternoon. The patients were kept for a night post operatively and seen in the wards prior to discharge. We worked with surgical trainees as well as a local pediatric surgeon and urologist to collaborate on some of the cases. We also assisted the local surgeons with some emergency cases including a splenectomy, amputation, and trauma laparotomy. There were no complications and the surgical trainees have been asked to keep us informed of any developments.












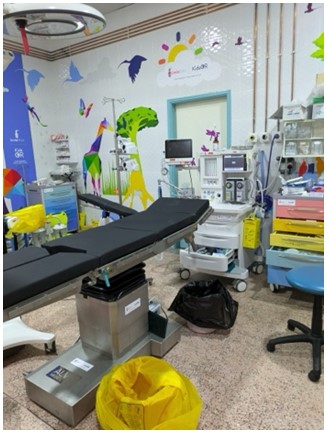
OR staffing was limited and often consisted of learners or students without any real guidance or oversight. The physical ORs were in decent condition with electricity, battery powered lights and anesthesia machines in three rooms. The upstairs ORs had been renovated and decorated by KidsOR and the fourth OR was in the process of being equipped and stocked. There is laparoscopic equipment available and interest by the surgeons in future laparoscopic camps. The OR provided drapes, gowns, and sterile instruments although gowns and drapes were at times the limiting factors for being able to get through a full day’s list.



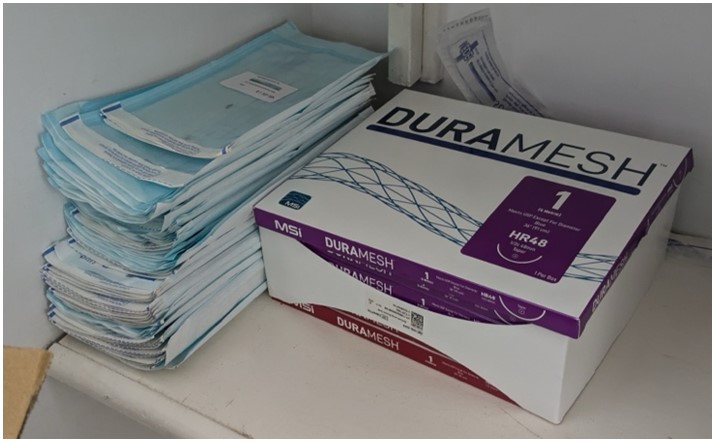
The Ministry provided transportation support as well as tea and lunch every day for the team and the entire OR staff. We had our fill of Kenyan tea and delicious local food. The Ministry also came with higher level support during the second week for a ceremony and tree planting at the hospital. Our donated supplies were also presented at this time. We left the mosquito net meshes that were not used for the hospital as well as donations of Duramesh.




Social Activities:
Our evenings were spent walking from the hospital, resting, and enjoying local restaurants and libations. Over the weekend Peter was gracious to come to Meru from Nairobi and played Tour Guide. On Saturday we went to Ngare Ndare Forest Park where we did some off-road driving, hiking to waterfalls which were brown in the rainy season but usually are a beautiful clear turquois, and walked across a canopy walk. On the way home we drove through the Lewa Wildlife Conservancy where we saw Zebra, ostrich, rhino, elephants, and a giraffe amongst other local animals. On Sunday we drove a bit further to get to Meru National Park, the least visited Park in Kenya, and went for a six-hour game drive with some good showings but no cats.




Advice for future teams:
There is good opportunity for collaboration in Meru. The hospital is well run, and the surgeons are friendly and competent but obviously lacking time and resources to do much outside of emergency cases. I believe many of them also have private practices in other hospitals. The trainees are used to a level of autonomy that is not the norm in US hospitals, so although they were interested in learning they were not used to our level of supervision. Planning with the hospital and OR staff will help to ensure a patient load that keeps the Hernia International Surgeons busy but doesn’t overwhelm the hospital capacity. There is room for improvement or growth in the patient recruitment as well as in the use of local and spinal anesthetics and early discharge home. The operating theater could be better optimized in its efficiency of use and its sterilization and hygiene practices. Having additional nursing staff with the team would be helpful as well.
** For supplies being brought into country, we came across some difficulty with customs even with the supplies marked as donations for humanitarian use. They are sensitive to medical supplies and expired supplies. If working with Peter Karanje or the ministry, send him a list of supplies and you may be able to avoid this with a letter of support. **
Heid Miller, MD MPH
Maine, USA


